
The Nicotine Fix
America’s cigarette addiction may seem to be mostly over. But low-income Americans continue to smoke—and die—at alarming rates. A radical new strategy could help them quit once and for all.
A custome lothsome to the eye, hatefull to the Nose, harmefull to the braine, dangerous to the Lungs, and in the blacke stinking fume thereof, neerest resembling the horrible Stigian smoke of the pit that is bottomelesse.
—King James I, A Counterblaste to Tobacco, 1604
Humans take great pride in the fact that we dominate all other species with our sophisticated cognition. Yet while virtually all other species instinctively flee from smoke, we choose to suck it into our lungs. Worldwide, that one lapse in intelligence—inhaling tobacco smoke—costs us 6 million members of our species annually, while causing another 120 million or so to suffer from intractable lung, heart, and other diseases. Tobacco is now on pace to take one billion lives over the 21st century.
It’s been 50 years since Surgeon General Luther Terry released Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. That event ranked among the top news stories of 1964—a year that saw Lyndon Johnson’s election, the Civil Rights Act’s passage, Freedom Summer, and the Gulf of Tonkin Resolution. The report confirmed that cigarette smokers have a 70 percent increase in mortality. It linked smoking with lung cancer, emphysema, and heart disease. It also found a positive correlation between smoking pregnant women and underweight newborns.
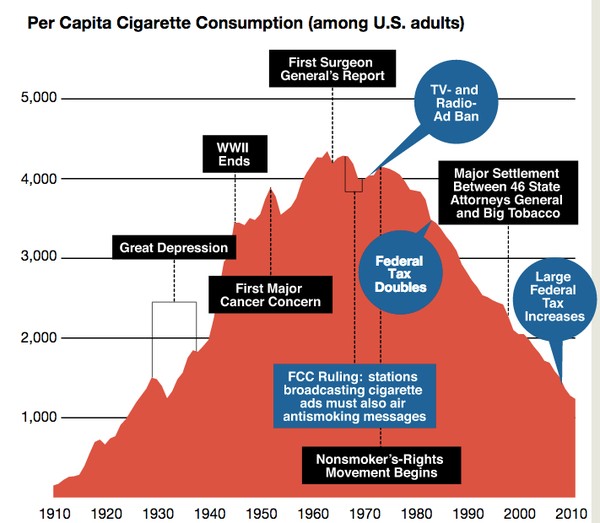
It’s hard to overstate the impact of this report. During the first six decades of the 20th century, smoking had grown from a casual pastime to a national addiction. In 1900, the average American adult smoked just 54 manufactured cigarettes each year. Then, in 1913, the R.J. Reynolds Tobacco Company introduced Camel cigarettes in what many consider to be the first modern advertising campaign. Shortly thereafter, cigarettes went to war. Before World War I, cigarettes were considered effeminate—manly men smoked cigars and pipes and used chewing tobacco. But in the trenches of Europe, soldiers did not have time to pack a pipe or savor a slow-burning cigar. Cigarettes were included in doughboys’ rations as they shipped off to Europe. Soldiers came home addicted to what Henry Ford called “the little white slaver.” Consumption increased rapidly after that, and by 1963, the average American was smoking 4,345 manufactured cigarettes per year.
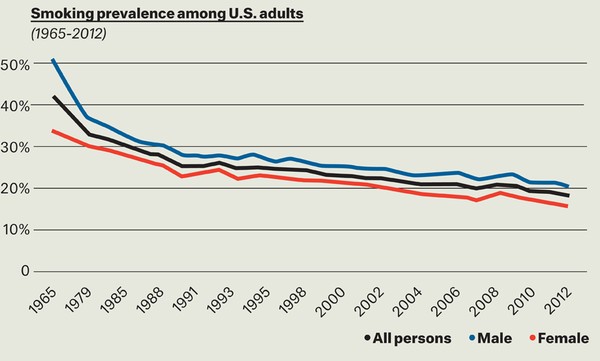
Then, after Surgeon General Terry’s announcement, cigarette use suddenly began to decline. With only a handful of early exceptions, it has continued to decline annually ever since. Both the rise and fall of the cigarette were so dramatic that Harvard historian Allan Brandt dubbed the 1900s “The Cigarette Century.”
The 1964 report launched an era of tobacco control—a series of public- and private-sector interventions that, taken together, have averted an estimated 8 million premature American deaths. On average, each of these 8 million beneficiaries gained two full decades of life. It’s not hard to see why the Centers for Disease Control and Prevention included tobacco control on its list of 10 great public health achievements in the 20th century.
Smoking is rarely tolerated in white-collar workplaces. Half of all states prohibit smoking in offices, restaurants, and bars. In hundreds of parks and beaches throughout the country, smoking is verboten. Among college-educated, upper-middle-income Americans, tobacco addiction is far from the epidemic it once was. Most of them don’t smoke, and neither do their friends. In those circles, the problem may seem to have been solved.
The problem has not been solved, however. Forty-five percent of all Americans who completed a GED continue to puff away. The habit also persists for over 30 percent of American Indians and Alaska Natives. Perhaps most vexingly, smoking is rampant among the nearly 40 percent of the population with diagnosable psychiatric disorders; they smoke at a rate almost double the national average. Cigarettes continue to claim the lives of 480,000 Americans each year, accounting for one of every five deaths in America.
To put these numbers in perspective, consider the Pink Ribbon campaign that has mobilized millions of Americans to contribute to the battle against breast cancer. It’s a worthy battle by any measure. Yet how many people, even highly educated people, realize that 82 percent more American women now die of lung cancer than die of breast cancer?
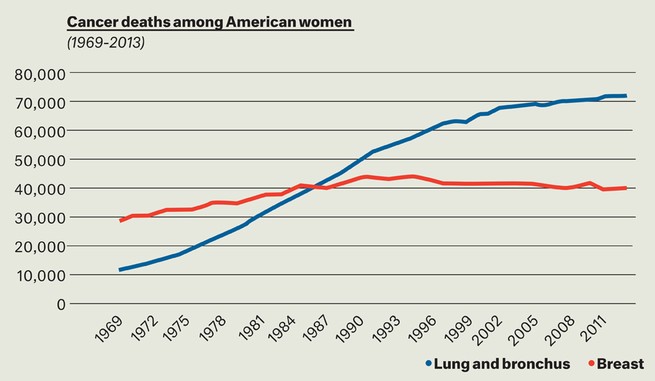
Why is there no Brown Ribbon campaign to combat cigarette smoking? We fear that the answer lies in the fact that smoking is largely a low-income problem, and the resulting illnesses and deaths are often blamed on the victims. In certain circles, cigarettes are not only common but practically ubiquitous. Yet for those who run the nation’s businesses, those who shape its policies, those who fundraise, blog, and tweet, those who read and vote in the highest numbers, the issue has largely disappeared from view.
It took 40 years—from 1965 to 2005—to halve the rate of cigarette use. Today, somewhere in the range of 18 to 20 percent Americans smoke, depending on which national survey one reads. Will it take another 40 years for the rate to halve again?
It looks that way, based on a model one of us (Warner) has been developing with the University of Michigan’s David Mendez. The model, which we’ve been testing since the 1990s, has proven quite accurate thus far. Its predictions are sobering. Based on the rates at which people start and stop smoking—the latter hasn’t changed much in decades—it will take us until 2050 to come close to a national smoking prevalence of 10 percent. Ten percent sounds pretty good in light of both history and today’s numbers. But consider that 10 percent prevalence in 2050 implies that there will be hundreds of thousands of entirely preventable premature deaths from smoking every year.
Unfortunately, it will not be enough for public health professionals to push harder for the same approaches that have worked so far. The decline of the past few decades has largely been accomplished through mandating smoke-free workplaces in half of all states, increasing cigarette excise taxes in nearly all states, mounting effective media campaigns, and imposing restrictions on tobacco company marketing. To cut smoking prevalence in half again in fewer than 40 years will take something more than these evidence-based tools of the trade.
What is that “more”? The answer depends on whom you consult. Simplifying considerably, one can roughly divide the tobacco control community into three groups. The solutions championed by each group are not mutually exclusive, although listening to their most ardent proponents you might be forgiven for thinking so. As we will see, none of them can solve America’s smoking problem on their own. Collectively, however, they may have found the answer. They just don’t know it. These groups are the Traditionalists, the Harm Reductionists, and the Endgamers.
The Traditionalists: If It’s Working, Keep Doing It
The Traditionalists are the largest group within the tobacco-control community. These veterans of the tobacco wars witnessed the remarkable progress wrought by the arsenal of evidence-based interventions noted above. These weapons have been able to beat back a tobacco industry that uses its economic might to pull strings in Congress and every state legislature. While the giant has not yet been slain, it has suffered serious wounds.

The Traditionalists believe that if we just do more with these weapons, we will continue to achieve remarkable progress. They want to jack up cigarette prices higher and higher, push the 20-some laggard states to adopt smoke-free workplace laws, and extend smoke-free coverage to public parks, beaches, university campuses, and public housing. They want to see more large, creative, counter-advertising campaigns like the CDC’s Tips From Former Smokers, in which real people share their cigarette-related horror stories.
All of these approaches have been proven to work. Traditionalists often point to California, one of the first states to adopt these measures, where smoking prevalence now stands at 12.6 percent, the lowest in the nation outside of Mormon Utah. In New York City, another oft-cited example, former Mayor Michael Bloomberg made aggressive use of these traditional tools, driving smoking down rapidly and substantially among both teenagers and adults.
Traditionalists must face a discomfiting fact, however. These conventional interventions will continue to bring progress—but slowly, and only up to a point. Substantial tax increases, one of the most effective interventions so far, eventually will come up against a political and moral stone wall: the inequity associated with a regressive cigarette tax. The majority of smokers are poor. They are more price-sensitive than the rich, and when they’re confronted with higher prices, they do quit in larger numbers than wealthier smokers do. But whether rich or poor, only a minority of smokers quit because of increased costs. That means most poor smokers continue to smoke when the cigarette tax goes up, and the financial burden they bear as a result is heavy indeed. So while we would like to see high overall prices on cigarettes, there are clear limits to this approach.
Consider a married couple with a $30,000 a year income. If each spouse smokes a pack a day and they live in a state where cigarettes cost an average of, say, $6.00 a pack, they will devote 15 percent of their very limited income to cigarettes. Six percent of their income will go to cigarette taxes alone. If they live in New York City, the city’s new minimum price per pack of $10.50 will drain a full quarter of their income. Some low-income New Yorkers surely pay more in tobacco taxes than they do in taxes to support Social Security and Medicare.
Other evidence-based weapons in the Traditionalists’ arsenal have limits, too. Half of all states already mandate smoke-free workplaces; in other states, individual businesses have established smoking bans as a matter of company policy. There are only so many more workplaces that can go smoke-free. Some states have adopted additional smoke-free policies—for instance, banning smoking in cars when kids are present. But to bring about a huge leap in progress, such policies would have to extend well beyond their current and readily defensible limits. Smoking might have to be banned on all city streets, for example, and perhaps even in non-workplace private properties like the home, a proposition no one but a handful of Prohibitionists/Abolitionists would support (more on them later).
Large counter-advertising campaigns constitute another major evidence-based intervention. These require (and deserve) substantial funding and virtually constant creative renewal. Fortunately, this year will witness a barrage of tobacco control media campaigns coming from the federal Office on Smoking and Health, the Food and Drug Administration, and the American Legacy Foundation. But how long will cash-strapped federal agencies be able to fund such programs? Even now, the American Legacy Foundation is digging into its endowment to fund its campaign.

The latest innovation in tobacco control—large graphic warning labels—should have festooned cigarette packs in September 2012. But their adoption was forestalled by industry legal action. If these labels do eventually become law, research suggests that they will decrease smoking, but the benefits may prove modest. And the ever-resourceful cigarette industry—and resourceful smokers—can always find ways to hide these unpleasant reminders, for example by repopularizing the old-fashioned cigarette case.
The Harm Reductionists: An Alternative to “Quit or Die”
Harm reduction is simple in concept but controversial in practice. Instead of eliminating a given risky behavior, proponents of this idea seek to reduce the dangers involved—often by substituting a closely related, less-dangerous behavior. Examples abound: Offer chronic heroin users clean needles and methadone treatments. Instead of requiring abstinence-only education, teach students about birth control and, in some school jurisdictions, provide free condoms.
We know from research that many of these approaches work. Provision of clean needles has markedly slowed the spread of HIV in many nations. The designated driver campaign, perhaps the most successful contemporary use of harm reduction, has substantially reduced traffic fatalities by addressing drunk driving rather than alcohol consumption itself.
Some cigarette smokers very much want to quit, often desperately so, but simply find complete deprivation intolerable. Enter tobacco harm reduction (THR), the idea that some smokers can wean themselves off cigarettes—by far the most dangerous form of tobacco consumption—by switching to alternative nicotine or tobacco products.
Many anti-smoking advocates view such approaches with extreme skepticism. The two most prominent “harm reduction” efforts—created by the tobacco industry itself—caused tremendous harm.
The first was the filtered cigarette, which accounted for just 1 percent of all cigarette sales in 1950. That was the year the first scientifically robust study identified smoking as a cause of lung cancer. When these findings were publicized in the media—most notably in a December 1952 Reader’s Digest article entitled “Cancer by the Carton”—the first widespread smoking-and-cancer scare enveloped the nation. Smoking rates plummeted for two years as people scrambled to quit.
The industry responded by producing and heavily advertising filtered cigarettes, claiming that they let the flavor through while trapping the “bad stuff.” (The industry never specifically admitted that smoking caused lung cancer, or any other disease.) Kent, the first successful brand of filter-tipped cigarettes, was promoted as “the one cigarette that can show you proof of greater health protection.” It utilized an “exclusive Micronite Filter” that, ironically, was made of crocidolite asbestos.
Industry documents, subsequently made public as a result of tobacco lawsuits, reveal that the industry never truly viewed filtered cigarettes as less dangerous than unfiltered cigarettes. Rather, it viewed the filtered cigarette as a means of assuaging the public’s fears. Still, many people fell for the sales pitch, desperately seeking reassurance that it was okay to smoke. Smoking resumed its upward trajectory in 1955, and by 1960, filtered cigarettes dominated the market.
A second public scare in the late 1960s and early 1970s generated another industry innovation. After millions of people became concerned about the widely publicized toxicity of tar and nicotine (often conjoined in the public’s mind), cigarette companies introduced a wide variety of low-tar-and-nicotine (low t/n) cigarettes. The design of these cigarettes was brilliant. One of the most common features involved a ring of tiny perforations around the filter tip. The government’s cigarette testing machines, intended to assess tar and nicotine yields, held cigarettes at the very tip end and puffed on them with a constant force at regular intervals. When the machine “inhaled,” the perforations allowed air to enter the cigarette, thereby diluting its yields of tar and nicotine. The government’s widely reported measures showed often very large reductions in emissions.
People did not smoke like the machines, however, and the industry knew it. Smokers held the cigarette in the middle of the filter tip, thereby occluding half of the ventilation holes. Smokers with large lips, referred to in the trade as “congenital hole-blockers,” might cover 100 percent of the perforations. For flesh-and-blood smokers, tar and nicotine yields were considerably higher than those recorded by the government’s testing machines.
Once again, industry documents show that low t/n cigarettes were public relations devices, designed from the beginning to allay the public’s fears. One prominent 1975 ad for True cigarettes shows a woman reflecting, “I thought about all I’d read and said to myself, either quit or smoke True. I smoke True.” These ads worked fabulously: Millions of Americans switched to low t/n cigarettes, many likely in lieu of quitting.

Most smokers found the low t/n product less satisfying than full-strength cigarettes. Struggling to get their accustomed levels of nicotine, low t/n smokers engaged in all kinds of compensatory behaviors, puffing harder or more frequently on their cigarettes, smoking them closer to the butt, and smoking more of them.
In a 1983 study, levels of cotinine, a derivative of nicotine, in smokers’ blood showed little to no correlation with the machine-measured nicotine yields. Smokers of low t/n cigarettes displayed lung cancer rates similar to those among people who smoked regular-yield cigarettes. The only real difference was that low t/n smokers developed cancers further down into the lung, apparently as a result of drawing harder on their cigarettes.
Thus, the two most successful entrants into the “harm reduction” market were not harm-reducing at all. Quite the opposite: They offered an attractive way to continue smoking to millions of frightened smokers who otherwise might have quit.
In the 1980s, R.J. Reynolds did attempt to market an apparently genuine lower-risk alternative to cigarettes, investing hundreds of millions of dollars in a product called Premier. Designed to look like a cigarette on the outside, Premier really was tobacco rocket science for its era. Small beads impregnated with nicotine were enclosed in an aluminum capsule inside the rod of the device. When the user lit the carbon tip with a cigarette lighter (because a match didn’t burn hot enough to ignite it) and sucked on the “filter tip” end, the heat evaporated the nicotine on the beads, allowing the user to inhale nicotine and glycerine.
The aluminum capsule was held in place by tobacco, even though no tobacco was actually consumed. The patent, which described the product as a nicotine-delivery device, noted that the tobacco in the product was optional; the capsule could have been held in place by any number of other means. Apparently the purpose of including the tobacco was legal: The device looked like a cigarette on the outside and included tobacco inside; therefore, the industry could argue that it was a cigarette (even if it wasn’t) and should thus be exempt from the usual FDA drug delivery device regulations.
Premier failed to impress consumers when RJR test-marketed it in 1988. Six years later, RJR test-marketed a similar product called Eclipse, which used a simpler system designed to generate a more pleasing taste and smell. That failed, too.
Despite this unpromising history, the current generation of THR products may be different, and more beneficial. For one thing, many modern products were developed not by the cigarette industry but by entrepreneurs seeking to compete with the industry. Until recently, those alternatives consisted primarily of pharmaceutical nicotine products (used on a long-term basis, not merely as a short-term aid to quitting) and an assortment of smokeless tobacco products. Many of these products likely served as an effective harm-reduction for a subset of nicotine consumers who otherwise would have continued smoking. At times, health authorities have overstated the dangers of smokeless tobacco. For example, the federal government frequently told the public, “Smokeless tobacco is not a safe alternative to cigarettes.”
It’s true that smokeless tobacco is not entirely safe, but even products high in nitrosamines—an element believed to be highly carcinogenic—present a much lower risk than smoking. In the case of newer low-nitrosamine smokeless products, research suggests that the risk is no more than 10 percent that of cigarette smoking, and possibly much less. If smokers substituted one of these products for cigarettes—assuming they would not quit otherwise—their health gain would be immense.
The problem is that these products may sustain cigarette use among people who would otherwise quit. This concern has intensified with the new-found popularity of electronic cigarettes, commonly known as e-cigarettes, and other ENDS (electronic nicotine delivery systems). A prominent Wall Street analyst believes that e-cigarettes will constitute half of the cigarette/e-cigarette market in less than a decade. Some Harm Reductionists appear to believe that e-cigs are the solution to America’s cigarette problem. Unlike Premier or Eclipse, many brands of e-cigarettes are marketed by companies that have no ties to the tobacco industry and, in fact, openly seek to undermine it. One major brand, NJOY, has the stated mission “to obsolete cigarettes.”
E-cigarettes are not cigarettes at all. Rather, they are (mostly, not all) cigarette-shaped devices that use batteries to heat a liquid mixture containing nicotine and propylene glycol, which creates the smoke-like vapor upon exhaling. Users—known colloquially as “vapers”—suck on the device and draw in vaporized nicotine, along with selected flavorings and often a few additional chemicals.
Users often believe they are inhaling nicotine into their lungs, as with conventional cigarettes. In fact, only a subset of e-cigarettes deliver significant amounts of nicotine to the lung. Many merely deposit nicotine on the linings of the mouth and throat, creating a slow absorption into the bloodstream, not unlike other smokeless tobacco products, and nicotine gum. This slow absorption delivers less nicotine “kick”; hence, many e-cigarettes are less addictive than cigarettes. But they’re not non-addicting.
The most pressing concern about e-cigarettes and other THR products is that smokers will use them to tide themselves over during periods when they can’t smoke, for example while they’re at work. By sustaining their nicotine blood levels, the products will actually keep their addiction going, and they’ll continue to use cigarettes the rest of the day. Were the alternative products not available, the argument goes, these smokers would be more likely to quit altogether. Research has established, for instance, that smoke-free workplace policies increase quitting.
Critics of THR worry about other possibilities, too. Using smokeless products might cause former smokers to relapse. Kids who avoid cigarettes might experiment with e-cigarettes, quite possibly eventually moving on to cigarettes to get a bigger kick. What’s more, the new “safer” smokeless products may not be safe. The public health community is divided on this question: Many (though few with specific THR expertise) believe that smokeless products are so dangerous in and of themselves that encouraging their use in lieu of cigarette smoking would be akin to encouraging people to consume arsenic instead of hydrogen cyanide (each of which, incidentally, is present in cigarette smoke). The problem here is a lack of definitive evidence. So far, the research hasn’t given any clear indication whether using these alternative products will increase or decrease the net population harm associated with cigarette use. Our own risk-calculus leans in the direction of supporting harm reduction.
Consider a striking natural experiment in Sweden. For several decades, a sizable proportion of the Swedish male population has been using snus, a moist tobacco powder with relatively low nitrosamine levels. Sweden also has the lowest rate of male cigarette smoking in Europe, likely due to the country’s heavy taxation of cigarettes and its low taxation of snus. And Sweden boasts Europe’s lowest male lung cancer death rate—as well as the lowest male death rate from smoking-related cardiovascular diseases, and the lowest male death rate from other cancers that are attributable to tobacco. For men between the ages of 60 to 69—a prime time for smoking-related deaths—the tobacco-attributable death rate in Sweden is 40 percent lower than the next-lowest tobacco-attributable death rate among EU countries. Swedish females, apparently not as enthusiastic about snus, have cigarette smoking rates—and tobacco-related death rates—similar to those of women in the rest of the EU.

Swedish men are not shy about using tobacco. Their overall tobacco consumption is actually higher than that of males in most western nations. Yet their smoking rate is very low, and extensive research has found little evidence that sustained use of snus causes any serious health problems, including cancer.
The Holy Grail of cigarette substitutes might well be a true pulmonary inhaler that delivered only nicotine (and perhaps some flavorants) into the lungs. A true pulmonary inhaler would be highly addictive, possibly as addictive as cigarettes, but without the severe health risks that come with inhaling smoke. (Many members of the public believe nicotine to be the dangerous element in cigarette smoke. It isn’t. The principal danger associated with nicotine is its addictiveness, which keeps people inhaling scores of toxic chemicals in cigarette smoke.)
Enter Dr. Jed Rose from Duke University. A co-inventor of the nicotine patch and long-time, well-respected smoking cessation researcher, Rose developed a device that carries nicotine directly into the lungs, accompanied only by pyruvate, a substance already in our bodies. Rose tried to sell his patent to major pharmaceutical companies, but none of them bought it. We suspect that these firms did not want to be associated with selling an addictive substance, especially one with a reputation as unsavory as nicotine’s.
Rose eventually offered the patent to Philip Morris International (PMI, not to be confused with Philip Morris USA). PMI bought the patent and announced last year that it intended to test-market a new product—one that sounds suspiciously like Rose’s inhaler—during the next few years, possibly in Europe.
Although e-cigarettes and other smokeless products are likely to benefit individual smokers, we do not believe that any of today’s THR options have much potential to greatly reduce smoking rates. In a different environment, they might make a significant contribution. More on this after we take a look at the final group of tobacco control advocates: The Endgamers.
The Endgamers: Drastic Times, Drastic Measures?
Frustrated with the slow pace of smoking reduction, a third group has emerged within the tobacco control community. Their radical approaches have come to be labeled tobacco endgame policies.
The largest group of endgame proposals includes variations on prohibition. One, developed by academics in Singapore, calls for prohibiting the possession of tobacco products by anyone born after the year 2000—creating a so-called tobacco-free generation. The Australian state of Tasmania is currently considering adopting this as policy.
Another strategy, originating in New Zealand, involves gradually cutting off tobacco supply by increasing quotas on sales and imports. (Because New Zealand is a relatively small and isolated island, smuggling is less of a concern than it is in the United States.) In 2011 the New Zealand government committed to becoming smoke-free by 2025, which it defined as a national smoking prevalence below 5 percent. As it considers more radical proposals, the country is making use of traditional measures, such as further raising tobacco taxes and restricting smoking in more and more areas.
Smoking prohibition in itself is not a new idea. In the early 1600s, when Ottoman subjects were beginning to take up tobacco smoking, Sultan Murad IV adopted the most draconian tobacco-control policy of all time: He declared smoking punishable by death. He is reported to have enforced his policy by having smokers “drawn and quartered by four strong horses”—thus providing the first definitive proof that smoking is bad for your health. Because the draconian policy did not stop his citizens from smoking, however, he also offered the first incontrovertible evidence for the seductiveness of nicotine.

Smoking prohibition also has a precedent in the United States. Between 1890 and 1927, 15 states banned the sale of cigarettes. In at least one state, resourceful cigarette companies evaded the ban by selling matches, packaged along with a “free” pack of cigarettes. All of the bans were eventually rescinded in response to pressure from the industry. Many states and localities rely upon tobacco revenues. If cigarettes were banned today in a given state, smuggling would be pervasive across close, completely unguarded borders, and the state would risk additional lost revenue (and jobs) as smokers purchased other items when crossing borders for cigarettes. Still, it would be perfectly legal today for individual states or local communities to ban the sale of cigarettes, or even smoking itself.
Until now, few American public health professionals have been willing to openly discuss prohibition. The most direct call comes from Stanford historian Robert Proctor, who presents a compelling case in his recent history of smoking, Golden Holocaust: Origins of the Cigarette Catastrophe and the Case for Abolition. Proctor argues that abolition (a term he prefers to prohibition) would reduce healthcare costs, increase workforce productivity, reduce the incidence of fires and environmental damages, and cut out a source of longstanding corruption. He also argues that nicotine addiction actually robs smokers of their free will, and that eliminating cigarettes would increase, rather than decrease, their liberty. Such reasoning might have seemed far-fetched in the past, but recent Gallup surveys show that one fifth of Americans favor a complete ban on smoking—nowhere near a majority, but a significant enough number to legitimize the conversation.
No state is likely to abolish cigarettes anytime soon. Any such efforts would almost certainly be stymied by smokers, cigarette retailers, and the politically influential tobacco industry. Opponents also fear that negative side-effects of prohibition, including underground markets, would outweigh the benefits. America’s deep libertarian ethos also resists the idea of banning a largely self-harming product. (Secondhand smoke is a separate concern, and it can be largely addressed by prohibiting smoking in public spaces.)
A more nuanced approach involves reducing the nicotine in cigarettes to the point where it’s no longer addictive. This proposal was first put forward by Drs. Neal Benowitz and Jack Henningfield—two of the world’s leading experts on nicotine addiction—in a 1994 article in the New England Journal of Medicine. Public health specialists view the Benowitz-Henningfield proposal with considerable interest, and The Family Smoking Prevention and Tobacco Control Act of 2009 gave the Food and Drug Administration the authority to set it in motion. The law doesn’t allow the agency to ban nicotine from cigarettes altogether. But it permits the FDA to establish performance standards—which means it can require tobacco companies to reduce nicotine delivery levels, to the point where experts believe cigarettes will no longer be capable of sustaining addiction. Research is currently underway to evaluate whether this would work. If the FDA decides to adopt the regulation, it could extend it to cover all combusted tobacco products. This provision is important, because an ever-creative tobacco industry would likely circumvent nicotine reduction in cigarettes by promoting “little cigars” or other combustible products.
Conversations about cigarette regulation come at a most ironic time, as more and more states are beginning to legalize marijuana. But these considerations may soon prove relevant for marijuana smokers as well. The legalization of cannabis presents an especially intriguing opportunity for the e-cigarette business. E-cigarettes can be easily modified to deliver the psychoactive substance in marijuana in a pure form, thereby delivering the drug to the brain while avoiding smoke-related toxins. In fact, vaping is already a rapidly growing segment of the new legal marijuana market.
A Three-Part Solution
Earlier this year, Health and Human Services Secretary Kathleen Sebelius challenged Americans “to make the next generation a tobacco-free generation.” Perhaps eliminating all tobacco products should be the ultimate goal. Certainly the penultimate goal should be the elimination of tobacco smoking. To achieve that end, the three groups described above may need to commingle their principal ideas: traditional evidence-based interventions, harm reduction, and novel endgame strategies. The three groups don’t always talk with each other, and when they do the conversation often descends into acrimony. But each possesses a key ingredient of a highly promising three-step plan.
The first step will rely on traditional evidence-based interventions. Public awareness campaigns will continue to turn young people away from smoking and to encourage their elders to quit as they internalize the message that smoking is not socially acceptable. Smoke-free workplace laws will need to be adopted in all states that do not currently have them on the books. (Most of the states lacking them are in the South.) As public sentiment permits, smoke-free regulations should be extended to as many spaces as possible. State and (particularly) federal taxes should be raised substantially on cigarettes and loose smoking tobacco.

Taxes should not be raised on smokeless tobacco products and e-cigarettes. Too many tobacco control activists are eager to increase the taxes on cigarettes and other tobacco products equally. They shouldn’t be. Here’s why: Fully 70 percent of smokers say they want to quit. Yet only 2.7 percent succeed each year. Sure, there are smoking cessation pharmaceuticals available, and some health care professionals conscientiously counsel their patients about smoking. But to date, the combination of available drugs and health care counseling has yet to make much of a dent in the problem. We must recognize, and respect, that some smokers cannot (or will not) relinquish their nicotine. They may need something more. For them, the most effective help may include another method of nicotine delivery. Making sure these alternatives are lower-priced than cigarettes may make it more attractive for smokers to switch, as so many Swedish males have switched to snus.
The second element of the three-step plan involves effective regulation of smokeless products. That could (but would not necessarily) include prohibiting the most dangerous among them (presumably those delivering the highest levels of nitrosamines) while actually encouraging smokers who would not otherwise quit smoking to adopt the least dangerous alternative. The FDA could forbid marketing tactics aimed at non-tobacco users—children to be sure, but also adult non-smokers and former smokers — while promoting campaigns that specifically target current adult smokers who can’t (or won’t) quit to switch to these far less hazardous products. Manufacturers could be not only allowed but even urged to include an explicit and accurate health message: “This product has been determined by the Food and Drug Administration to be significantly less dangerous than smoking cigarettes.”
Once both of these steps are complete, the third step will be the pièce de résistance. It entails reducing nicotine yields from cigarettes and other combusted tobacco products to levels that will not sustain addiction. (An alternative—or perhaps additional—regulation would be increasing the pH of cigarettes and other burned tobacco to make inhalation far less palatable.) The availability, attractiveness, and relative low price of noncombustible nicotine alternatives will reduce the demand for illicit full-nicotine cigarettes, limiting the black market.
This mixed-modality tobacco-control regulatory strategy would have several huge advantages. It would not ban cigarettes—they could remain on the market, albeit with more marketing restrictions and without the addictive element that keeps so many smokers hooked. Americans will then have the freedom to inhale thousands of chemicals from burnt tobacco without the drug-induced compulsion to do so. For the very first time ever, people will be able to smoke precisely for the reason the industry always argued was their true motivation: for pleasure.
Will smokers persist in consuming cigarettes in the absence of a nicotine jolt? Most experts believe that the vast majority won’t. Some will. Perhaps we should agree that that’s okay. Those smokers will be making a free choice to consume a deadly product.
How about those who gravitate toward smokeless tobacco products and e-cigarettes? Will they remain addicted to nicotine? Some will; many others won’t. The question is: Should we care? The answer depends on whether you consider dependence per se to be dangerous. While nicotine use on its own may well present some health risks, few have so far been documented outside of pregnancy. Even then, nicotine used in a non-combusted form, as a means of avoiding cigarette smoking, is far less hazardous to a developing fetus than continuing to smoke.
Implementing this three-pronged plan will be exceedingly difficult, to say the least. It will require highly skilled maneuvering through the formidable bureaucratic maze of government regulation-making in general, and FDA regulation-making specifically. It will also demand political support from a courageous president and a Congress that places the welfare of citizens ahead of the financially driven election game. The tobacco industry would respond to any such proposal with aggressive lobbying initiatives and campaign donations, and it’s difficult to imagine Congress standing up to these efforts.
Even if this plan were to make it through the political and bureaucratic maze and be announced as policy, it would surely face years of tobacco industry litigation and other delay tactics. Ironically, this is the industry that promised the public in 1954: “We accept an interest in people's heath as a basic responsibility, paramount to every other consideration in our business … We always have and always will cooperate closely with those whose task it is to safeguard the public health.” That self-described “brilliantly conceived and executed” industry strategy was surely responsible for the deaths of millions of Americans.

Even today, the tobacco industry insists it has the public's health and wellbeing at heart. Last month, Reynolds American’s CEO, Susan Cameron appeared at Fortune’s Most Powerful Women Summit and made several bold statements. “People should quit,” she proclaimed. “Let’s try to find them some satisfying alternatives.” Cameron declared that her company was the leader in investing in lower-risk options like e-cigarettes and gum; on October 22, a spokesperson announced that Reynolds will soon ban smoking in its office buildings.
Perhaps it is too much to expect Reynolds to stop selling cigarettes while demand for the product remains. It is more reasonable to at least ask the company to stay out of the FDA’s way as it develops tobacco control regulations designed to improve the public’s health. Staying out of the way would mean refraining from lawsuits against proposed regulations, as well as behind-the-scenes efforts to block FDA regulation in Congress. Perhaps if Reynolds publicly pledged to use this restraint (and honored that pledge), Altria (Phillip Morris)—the company that has long portrayed itself as most supportive of public health initiatives—would feel compelled to follow suit. (Altria supported passage of the 2009 law granting FDA regulatory authority.)
All of this might sound like the tobacco-control equivalent of a pipe dream. But given nicotine’s addictiveness—and a behemoth industry’s unending campaign to push its principal product—it’s astonishing that we’ve made as much progress as we have. Since 1964, some 8 million Americans have each experienced an average of 20 additional years of life because they responded to tobacco control—the educational messages, higher prices, restrictions on advertising, smoke-free workplaces—by quitting smoking or by never starting in the first place. Thanks primarily to the decline in smoking, lung cancer rates are on the decline, and overall age-adjusted cancer mortality rates are falling, too.
For some Americans, anyway. According to the surgeon general, nearly half a million will succumb to a smoking-produced disease this year. Ten million will live with the ravages of smoking-produced chronic diseases. Some will be incapable of climbing a flight of stairs; some will be chained to oxygen tanks. And if nothing changes, 5.6 million of today’s children will join their smoking parents and grandparents in early graves.
Over a 50-year lifetime of smoking—say from age 15 to age 65—a pack-a-day smoker will smoke over a third of a million cigarettes. That means inhaling a toxic stew of some 7,000 chemicals 3.65 million times. In his 50th anniversary report, released earlier this year, the surgeon general calls for a rapid elimination of the use of all combusted tobacco products, which continue to threaten public health in such urgent and entirely preventable ways. If his vision is realized, it may well prove to be the single most important contribution to American health in the 21st century.
